This post is a long one, I pray you will still read it as it is worth it. Every CHD is different and every child with a CHD is different. There is always hope. This story is shared in two parts. Ashley's mom gave me permission to edit but I couldn't.
---------------------------------------------------------
June 7, 2010. I was booked for a repeat csection, after failing to progress while delivering my son, Thomas, almost three years earlier. We left for the hospital at 5:30 am. We were excited and nervous as all expetant parents are, first time or not.
I remember laying on the operating table waiting to hear that first cry. Suddenly, I heard it! My baby girl was here! They whisked her away to be cleaned off, and have her newborn tests administered. She scored a perfect ten on her APGAR - an achievement I'm told is quite rare.
Since our son was over 8 pounds at birth, I was shocked when they brought her over to me - she was so tiny! She only weighed 5 pounds, 15 ounces. She was a little string bean though, at almost 21 inches long!
We named her Ashley Louise. Ashley being a name that my husband Mark and I had always liked, and Louise being a family name on both sides. We thought it suited this dainty, beautiful little girl we had been blessed with.
The next morning a nurse came in with a doctor, saying they wanted to listen to Ashley's heart. The nurse said she thought she had heard a clicking noise the day before, after her birth. They both listened, but heard nothing abnormal, so I shrugged it off, too tired and sore to get upset.
The day progressed in a typical day-after-birth haze. Ashley was having a harder time breastfeeding than my son had. She would latch well, but fall asleep within minutes of starting. I chalked it up to newborn fatigue.
The next morning, 48 hours after Ashley's birth, the same nurse came back to listen to Ashley's heart again. This time, I knew something was wrong by the look on her face. She listened a second time, then turned to talk to me.
"Your daughter has a loud murmur in her heart." She went on to explain that this was a common occurance, that many babies had murmurs, but it didn't mean that anything was wrong.
"All the same," she continued, "I'm going to send the doctor up to see her." She left the room, and I lay there, stunned. I looked over at my beautiful daughter, sleeping in her bassinet, not ready to believe that anything could be wrong with her.
However, I did pick up the phone and call my husband, repeating what the nurse had just told me. I knew he was worried. He got our son ready for daycare, and then took the day off work to come be with me at the hospital, while we waited for the doctor. It was 8 am.
Thus started one of the longest days of my life. Visitors came and went, but we didn't mention our concerns. I know I barely even registered their visit.
Finally, at 7 pm that evening, the doctor came to see Ashley. We had waited almost twelve hours to find out if there was something wrong with our daughter's heart.
Dr. Mutrie, the doctor on call that day, looked her all over, listening carefully to her heart, and told us that she definitely had a loud murmur. He mentioned that sometimes they are caused by "holes in the heart", but reiterated what the nurse had said, that often, it's nothing. He was going to send the pediatrician up the next morning to see what he thought. He was sure it wasn't anything serious, since she was doing so well.
And she was. Aside from not nursing very well, she was perfectly healthy. She had great color, was very alert, and all her vitals were stable.
The next morning, when Ashley was 3 days old, the pediatrician, Dr. Mark Messenger, arrived to see Ashley. He did a thorough exam, and then questioned us about our family's "heart history".
He sat us down, and told us that he was very sure Ashley had a hole in her heart. He said it likely wasn't large, and that they are very common, often closing on their own. He went on to say that he was going to send us to a larger, regional hospital on hour away, where Ashley would undergo an echocardiogram, to diagnose her problems. The echo would be set up via live Telelink, with the IWK Children's Hospital. He would call us later that morning with the time. With that, he left. It was 10:00 am.
We were stunned. We were worried, but still trying not to blow things out of proportion until we knew what was going on. We received the call at 11:30, that we were to be at the hospital by 2:00 pm. My husband flew home to get things settled for my son, pack up my room and get everything into the car.While he was rushing around taking care of things, Ashley underwent her first cardiac test - an EKG. They had a hard time getting all the leads on her, since she was so small. The next challenge was getting her to stay still long enough!
I'm glad I had the foresight to ask the doctor for some pain medication for the trip. I was only 3 days post-surgery, and I was crammed into the backseat of our small Ford Focus, unable to move or change position. I was in misery, but no way was I not going with my daughter. At the Dr. Everett Chalmers Regional Hospital, Ashley underwent her first echo. When they were done, we were able to talk to the cardiologist at the IWK Children's Hospital, as well as the pediatrician, via teleconference.
They confirmed the shocking news that Ashley did have a Congenital Heart Defect, known as a VSD - ventricular septal defect. She had a "hole" in her heart, in the wall that divides her two lower chambers. Honestly, we really had no idea what that meant, or the significance of it.
We were given a few signs to watch for, told to call our doctor if there were any concerns, and sent home. We had several follow up appointments scheduled, including with cardiology, later that fall. The drive home was silent, with each of us lost in our own thoughts and worries. We called our family when we got home, but everyone was optimistic, saying things like, "Oh holes are so common, they're not a big deal!" It seemed everyone we talked to knew somebody indirectly that had a hole in their heart, and was just fine, they never had any problems with it.
It was falsely reassuring, and while I think they meant to be helpful, after later on, when things got worse with Ashley's health, I got tired of hearing it, because it felt like they were trivializing what we were going through.
We settled into our life at home. Ashley was still struggling with breastfeeding. She would latch on, start to suck, but then fall asleep quickly. She would only eat for 5 minutes, on one side only, and there was no waking her up to eat, once she fell asleep.
Aside from the difficulty breastfeeding, and jaundice setting in, the first week passed easily, and she appeared perfectly healthy. Our worry started to ease.
However, starting into the second week, we started noticing some different symptoms: her breathing rate seemed quite high, and her heart often felt like it was pounding when you held her. Her breastfeeding wasn't improving, and actually seemed to be getting worse. She often seemed like she was struggling to breathe while nursing. Ashley would latch on, start to suck and then pop off suddenly, almost gasping for air. She'd repeat this over and over, sometimes screaming after her gasps. It was so frustrating and worrisome for us.
The night before Ashley's two week check up, I was holding her, and could feel her heart pounding. This wasn't unusual, but what was alarming was how fast it was going. I counted the beats, but didn't believe my numbers. I counted again and again and again. I kept getting the same number: 200 beats per minute.
I called the hospital and they told me to get her to ER immediately. However, by the time we arrived at the hospital, her arrhythmia had stopped, and her rate was normal. While there, they decided to do a thorough check up anyways. First stop was the scales, where I was shocked to learn that Ashley had gained a full pound in only 6 days!
They hooked her up to the vitals monitors. Her heart rate had dropped into the upper limits of normal, though her breathing rate was a bit high, but no one seemed concerned.
The doctor came in and I told him about her VSD and what had happened with her heart rate. He commented that her belly looked quite swollen, and I told him about the rapid weight gain. They watched her vitals for approximately thirty minutes, and decided to let us go, since nothing appeared amiss. He sent us home after telling us that her heart rate had gone high likely because she was trying to have a bowel movement, and her belly was likely swollen from gas.
Ashley's check up was the next day. She was seventeen days old. We sat out in the waiting room and finally our name was called. I went into the room. There on the desk was a copy of Ashley's echo report. I read it while waiting.
I was shocked to learn that not only did Ashley have a moderate to large VSD, but she also had a second heart defect: a small ASD (atrial septal defect). I kept reading the numbers and figures, which made no sense to me, until I saw the following sentence in bold, and underlined:
Watch acutely for signs of congestive heart failure.
My stomach dropped, and suddenly I knew what was coming.
Only minutes later Ashley's family doctor came in. She scanned the report, listened to my account of what had happened the night before, some of the symptoms we'd been seeing at home, and then listened to her heart and breathing. She asked if we'd noticed any rapid weight gain. I told her about the 15 ounces in 6 days.
She left immediately saying to was going to make a call to Ashley's pediatrician, and would be right back. I barely breathed while she was gone, and was fighting back tears. It was a weird feeling - I knew what was coming, and yet was denying it at the same time.
She came back in only moments later and said, "Pack your bags and go, they're waiting for you." She told us she was sure that Ashley was in congestive heart failure, and she was sending us back to the regional hospital, immediately.
I remember leaving her office and falling into a chair in the waiting area, crying, while I tried to get Ashley back into her car seat. I was stunned. I called my husband and told him to leave work immediately and meet me at the doctor's office asap, so we could get our daughter to the hospital.
I remember looking at her, terrified. I didn't know anything about congestive heart failure. I knew that older people died from it. I kept looking at her, terrified she was going to die. Thankfully, I've since learned that that's not how congestive heart failure works.
We flew down the highway to the hospital, definitely breaking a few speed laws. My mind was working overtime. I kept thinking, "What did I do wrong?" I felt so guilty. I am the mother. I am the one that carried her, that formed her in my womb. I felt sure it was something I had done wrong.
Then I felt angry. "Why me?" I didn't drink, smoke or do drugs. I got regular prenatal care, took my vitamins plus an extra Folic Acid. Why not some crack-head who didn't care? And just as soon as those thoughts came, they vanished. Looking back, I know that is the first time I really felt God was with me. Instead, my thoughts took a new turn: "Why not me?". I had a loving, supportive husband. We had a wonderful network of family and friends. We had stable jobs and a solid roof over our head. While we sure didn't have a lot of money, we had enough to get by, pay our bills and have some left over for extras. I doubted any "crack-head" would be able to provide such a stable environment for a needing baby.
It was a real definitive moment in my life. I made the concious decision to leave my daughter's life in God's hands. To trust that He has a plan for her, for all of this. Good or bad, no matter what the outcome, He was and always is, in control.
We arrived at the hospital where the doctors confirmed that Ashley was in early stages of congestive heart failure. At that point they put her at a level of 3, on a scale of 1-10 for severity. They said they wanted to avoid her hitting a level of 7 or 8. She was started on a heart medication, a fluid pill called Lasix, and we were sent home.
I remember all of that so clearly. It's everything after that day, the rest of the summer and fall, that passes into a blur for me, because so much has happened. It has been a whirlwind of appointments, tests, hospitals, phone calls, emotions and fears.
Ashley continued to decline steadily until she was approximately 10 weeks old. Shortly after two weeks of age we had to start bottle feeding her, as breastfeeding was just too much work for her. We had to buy special bottles and nipples, ones that created the least amount of resistance, so she didn't have to work as hard to eat her food. Even with those measures she was only eating 12-15 ounces per day. Sometimes it would take us an hour just to get 2 ounces of formula into her.
By six weeks of age she was hardly gaining any weight, so the pediatrician started her on two more prescriptions, another fluid pill called Aldactone, and another medication to help strengthen her heart function called Digoxin.
He also started her on what's called "concentrated calorie" formula. Normal baby formula & breast milk is mixed so that for every ounce the baby drinks, they receive 20 calories. Ashley 's formula was now being concentrated to 27 calories per ounce, in hopes that she would start gaining some weight.
However, by nine weeks of age, she was officially diagnosed with "Failure to Thrive" - her weight had dropped completely off the growth charts. She was admitted to the Dr. Everett Chalmer's Hospital, which is an hour and a half away from our home. There she had an NG feeding tube inserted. We were taught how to administer her bolus feeds.
It was really difficult at first, as Ashley c0uld only tolerate tiny amounts of food at a time. On average that first week we had to feed her only 1 & 1/2 ounces, every 90 minutes, around the clock. It was draining. Thankfully, by the end of the first week, we had built her up to a full 2 ounces, every 90 minutes during the day, and every 3 hours at night. Mark and I would take turns getting up at 1:00 am & 4:00 am to feed her.
However, after only three days at home, she was re-hospitalized. A combination of the NG tube and her heart failure (which slows digestion) had caused her to develop reflux. Over twenty four hours she threw up every feed she took in, and ended up very dehydrated.
Back in the hospital, after she was treated for her dehydration, she was started on reflux medication, and they also changed her formula to one that was easier on her tummy.
Up until she was diagnosed with Failure to Thrive, open heart surgery had been talked about, but nothing definite said. They were more saying, "some day, maybe around a year of age". However, once she was diagnosed with FTT and the NG tube went in, surgery became a definite.
How do I describe what it's like as a parent to be told that your tiny baby, is going to require open heart surgery. It's the riskiest, most invasive surgery there is. Knowing that they would be literally stopping my daughter's heart to put her on bypass was terrifying. I tried my hardest to avoid even thinking about it, but every now and then I couldn't stop myself. I could almost picture her lying there, covered in tubes and wires with an incision down her chest. I could hear the alarm bells going off. I was terrified that something would go wrong. Those times, during those "day-mares", I cried and prayed and prayed for strength - and I always received it.
Ashley had a busy schedule. She had to have weekly blood work to check her electrolye levels. Her medications had the potential to throw them out of whack, which could cause her to have a heart attack or potentially fatal arrythmias. Blood draws were agnozing for her and me. Her veins were so tiny, it was common for them to be blown out during the draws, meaning they would have to start again and try another arm. Sometimes they couldn't get her veins at all, and would have to do heel pricks, which in a way was even worse because it took so long.
Then we had to worry about the sample hemolyzing (blood cells bursting, ruining the sample). Many times we were called back to the hospital because the sample had gone bad, and we'd have to put her through it again.
She had doctor's appointments every other week, and weight checks every week. Ashley has a large medical team following her which consists of: her family doctor, a pediatrician, her cardiologist and his nurse, a neo-natologist, two different dietitians, and Early Intervention.
There's just nothing I can say to make you realize how overwhelming, physically exhausting and emotionally draining this time was. Unless you've had a seriously ill child, you just can't imagine.
I admit, at times I would see a mother with her healthy baby, and feel jealous. Sometimes sad and frustrated. I guess you could say I felt sorry for myself. But not even so much for myself, as for Ashley, at the injustice of her having to go through all of this. Thankfully I never allowed myself to indulge in those feelings very long. I would just pray instead.
Around ten weeks of age, Ashley's heart failure started to stabilize. Her symptoms were being better controlled by her medications, and I think we began to breathe a little easier, as we counted down to her surgery, which we knew was going to be sometime mid-October.
However, around this time, she also developed a problem with high blood pressure. To this day, they're unsure what caused it. We had to take her on a rush trip down to the IWK Children's Hospital, which is six hours away from our home, where she underwent another echo, to make sure there wasn't another heart defect that they had missed. That came back okay.
They then put her through full kidney function blood work, as well as an ultrasound of her kidneys, to make sure there wasn't a different defect there. We were having to go to the hospital every day to have her blood pressure monitored, which at times was running very high. At one point, we were to see a doctor or the hospital every day (yes, even on weekends) for 14 days straight, sometimes twice a day for two or three different appointments. I was running on fumes and prayer at that point.
Thankfully, it seemed to resolve itself on it's own, and while we never did find out that cause, Ashley hasn't had problems with her blood pressure since.
Ashley started receiving Synagis vaccine shots which are a monthly immune-booster, to help her body ward off RSV. Almost all children have the virus by the age of 3. For most healthy children, it poses no problems, however, in children who are immune-compromised or have heart and/or lung disease, it can extremely serious. A simple cold for Ashley had the potential to turn into pneumonia.
I don't remember the day, but sometime in September, we received the call with the date for Ashley's surgery. I remember crying pretty well the rest of the day. We knew it was coming, but getting that call made it "real".
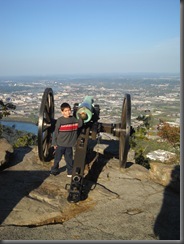
Aside from the NG tube in Ashley's nose, you would never suspect that she was seriously ill. She looked like any other healthy and happy baby, albeit tiny. It was easy to delude ourselves into thinking that it would be okay, that she would outgrow this, that it wasn't as serious as it is. That call changed that. There was no more pretending. It was real.
Those next few weeks my emotions were on a rollercoaster. I felt tense, angry, scared, exhausted, basically just a wreck, though so many people have commented on how strong I was, and how well I was holding it together. That was due solely to my faith in God, whom I cried out to daily.
Only three weeks before her operation, we were blessed to have a benefit breakfast thrown in Ashley's honor, to help with the growing financial costs. My husband's family put it on, and I will never
be able to thank them, or the community enough. The amount of people that donated food, money and their time for the breakfast was phenomenal. The amount of people that physically came to the breakfast and donated money was unbelievable. They had food prepared for 400 people, and they ran out, went out, bought more, and went through most of that.
Mark and I took turns going to the breakfast. When I walked inside our church hall and saw the place completely crowded with people there to support us, I started crying. I don't know that I had ever felt more overwhelmed, but in a good way.
Knowing that all those people, not just our friends and family, but complete strangers, were there for my daughter touched me in a way that I will never begin to be able to explain. It was humbling. It was to me, yet another proof of God's love, and that to anyone who doubts it, humanity at heart, is still good. I learned the true value and meaning of community and neighbour that day.
At Ashley's pre-op check up, only a bit less than three weeks before surgery, she was back in significant heart failure. Her weight gain had dropped again, she was starting to have difficulty breathing again, and her heart rate was fast and erratic. They doubled her medications in hopes of stabilizing her before surgery.
The week of surgery arrived, and we packed our bags for the six hour journey that would take us from our home for the next week to ten days. Thankfully we had several family members who were making the trip with us, not only to help us with Thomas, who was coming with us, but just to be an emotional support for us.
Ashley's surgery was set for October 21, 2010. Her pr-op day was set for October 20th, a day I will never forget. I remember waking up, with a mini anxiety attack. I couldn't believe that we were here, that we were less than 24 hours from her surgery. I was feeling panicked, and was doubting my ability to get through it. I was sick three times before we left for the hospital. I remember thinking, "If I'm this bad today, how am I going to handle tomorrow?"
We arrived at the hospital at 7:30 for a day scheduled full of pre-op testing for Ashley, and numerous meetings for us. She underwent three rounds of blood work, a chest xray and then a sedated study which consisted of putting Ashley under sedation, and then a detailed echo and EKG.
While she was in recovery, we were taken to another room where we had a meeting with various members of her surgical team. They went over step by step, the actual procedure, and all the risks - they left nothing out. We learned that she had between a 2-5% chance of dying, a bit higher than normal since she was less than 6 months old, and that she also had a higher than normal risk of requiring a pacemaker after surgery, due to where her VSD was located.
Then we were taken back to Ashley's room, where she was starting to wake up, and we had a meeting with her clinic nurse, who went over things like what to expect when we first saw her, explained about the ventilator she would be on, post-op care, what to expect when we got home etc...
The amount of information we received in those hours is mind-boggling. It was completely overwhelming, and at times it felt like we must be watching someone else's life. Surely, this wasn't our life? It wasn't our daughter they were talking about, was it?
And then we got the shock of our lives.